¹University of Calgary, Section of Ophthalmology, 7007 14 St SW, Calgary, AB, Canada, T2V 1P9 | ²University of Alberta, Faculty of Medicine and Dentistry, 8440 112 St NW, Edmonton, AB, Canada, T6G 2R7 | ³Mitchell Eye Centre, 5340 1st St SW, Calgary, Alberta, Canada, T2H 0C8
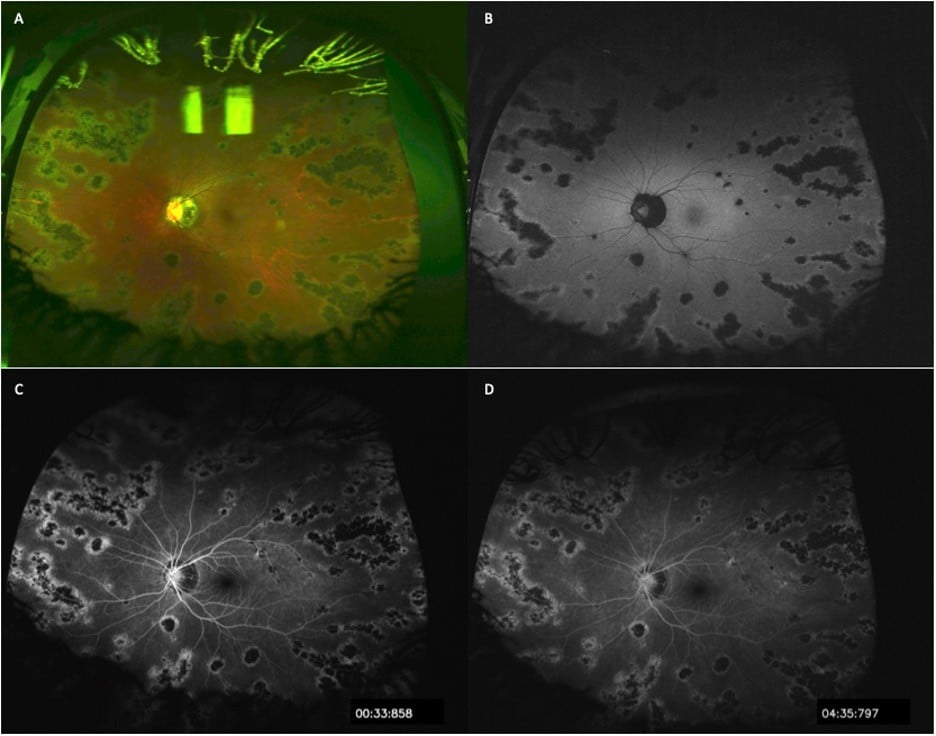
Figure Legend: A: Optos ultra-widefield color fundus photo OS with pigmented chorioretinal lesions following the retinal venous vasculature. The paravenous pigment extends to the periphery with sparing of the macula. Peripapillary pigmentation is present. The arteries, uninvolved retina, vitreous and optic disc are otherwise normal. B: Ultra-widefield Optos fundus autofluorescence photos OS with hypoautofluorescent, well demarcated, confluent patches following the retinal veins and corresponding to the pigmentary lesions observed in Panel A. There is mild increased autofluorescent signal surrounding the regions of retinal pigment epithelial migration. C: Fluorescein angiograms OS demonstrating hypofluorescent blockage regions along the venous circulation with surrounding hyperfluorescent staining. D: No leakage is observed in the late phase angiogram OS. Note that findings were equivalent and symmetric OD.
Case:
A 20-year-old middle-eastern female presented for a second opinion due to retinal findings noted on routine examination. She reported mild nyctalopia in both eyes. This was longstanding and an exact onset was difficult to ascertain. She was a healthy individual and did not take medications. Her family history was unremarkable. On exam, she had 20/20 vision bilaterally (OU). Fundus findings were symmetric OU with left eye (OS) findings presented. Optos ultra-widefield imaging revealed pigmented chorioretinal changes along the veins (Panel A). Ultra-widefield fundus autofluorescence demonstrates hypoautofluorescent corresponding areas with hyperautofluorescent borders (Panel B). Ultra-widefield fluorescein angiogram demonstrates hypofluorescent lesions with surrounding staining (Panel C). Late phase demonstrated no leakage (Panel D). Thorough workup including inflammation and infectious causes were negative. No progression has been noted.
Discussion:
Pigmented Paravenous Retinochoroidal Atrophy (PPRCA) is a rare condition classically diagnosed on routine examination due to the dramatic fundus findings, characterized by bilateral paravenous pigment accumulation along retinal veins with peripapillary and radial zones of retinochoroidal atrophy. Histopathological changes involve retinal pigment epithelium (RPE) atrophy with subsequent atrophy of the underlying choroidal layer.1 While the etiology of PPRCA is unknown, inflammatory and infectious causes have been reported.2 As such, differential diagnoses include inflammatory conditions causing chorioretinal atrophy and pigment migration, are important to consider in ruling out pseudo-PPRCA. A hereditary nature has been proposed, with few cases suggesting a familial occurrence.3 Most cases are sporadic. Patients are typically asymptomatic upon presentation, retinal findings without macular involvement tend not to affect visual acuity, and visual field and colour vision testing are usually normal. Typically, the posterior findings are isolated with an otherwise normal eye exam. PPRCA is a slowly progressive or non-progressive condition, with no specific treatment available to date.