¹Department of Ophthalmology and Vision Sciences, University of Toronto, Toronto, ON, Canada
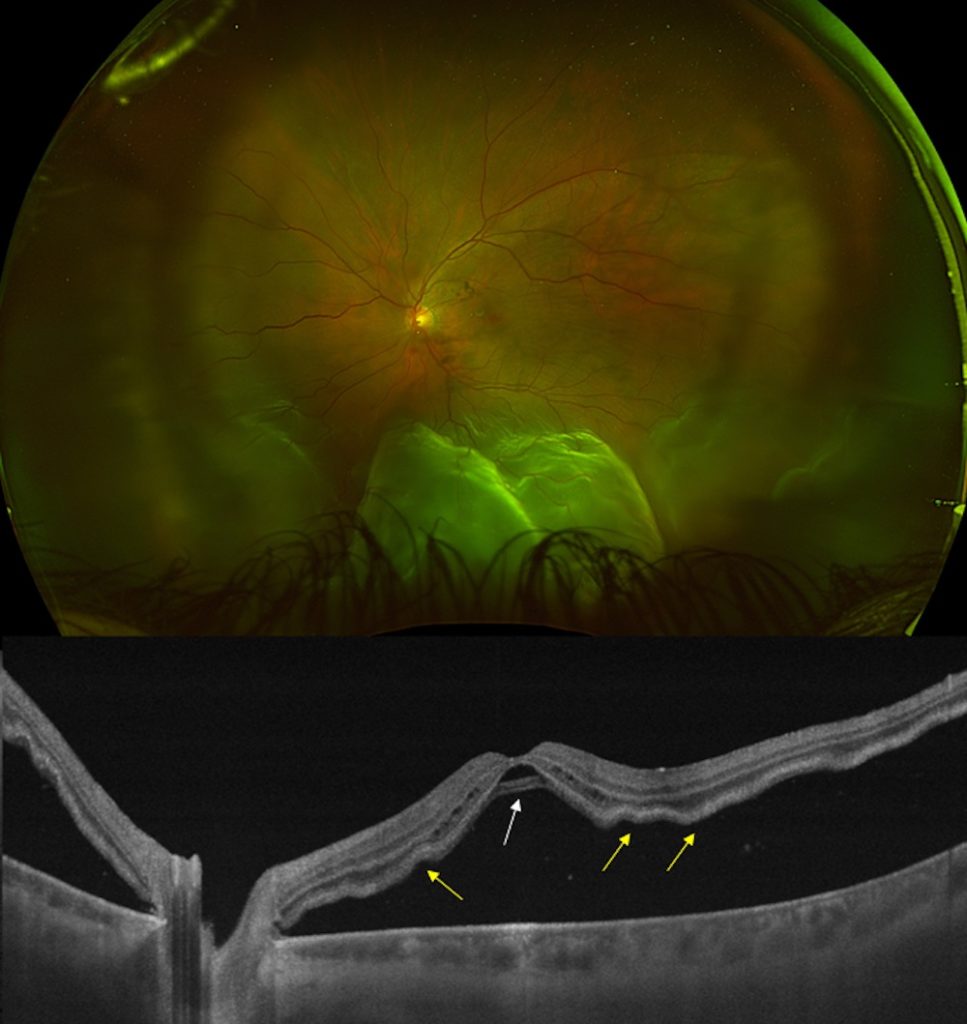
A 50-year-old male presented with a three-day history of central vision loss in his left eye. Visual acuity was 20/400 OS. Dilated fundus exam revealed a fovea-off rhegmatogenous retinal detachment (RRD). Swept-source optical coherence tomography (SS-OCT) confirmed a fovea-involving detachment with evidence of a bacillary layer detachment (BALAD) (white arrow) and mild outer retinal corrugations (ORCs) on the nasal and temporal parafovea (yellow arrows, see attached figure).
BALAD is an intraphotoreceptor splitting immediately posterior to the ELM within the inner segment myoid zone. SS-OCT hallmarks include: i) a split at the myoid creating a hyporeflective intraretinal cavity, ii) a hyperreflective granular band in the anterior border likely representing remaining cell fragments, and iii) a hyperreflective posterior border representing a continuation of the ellipsoid zone, presumably containing photoreceptor inner and outer segments.
BALAD was first described to be associated with RRD by Melo et al in 2022 in a prospective study of 93 consecutive fovea involving RRD. In RRD, the continuous influx of hypo-osmolar, liquified vitreous under the retina can cause ORC’s to form as a compensatory response to compressive forces generated from hydration and lateral expansion of the interphotoreceptor matrix. However, the unique arrangement of the Müller cell cone prevents the fovea from corrugating, which leads to stretching of the foveal bouquet. Further insult to the anterior wall of the BALAD cavity from adjacent cystic changes may result in a spectrum of BALAD-associated abnormalities that can culminate with the formation of a full-thickness macular hole. Specific SS-OCT features suggest that once BALAD forms, the fovea becomes susceptible to further injury due to areas of low-mechanical stability. Therefore, patients presenting with BALAD may benefit from timely management to avoid the progression to a full-thickness macular and, consequently, worse outcomes.