Department of Ophthalmology and Vision Sciences, University of Toronto
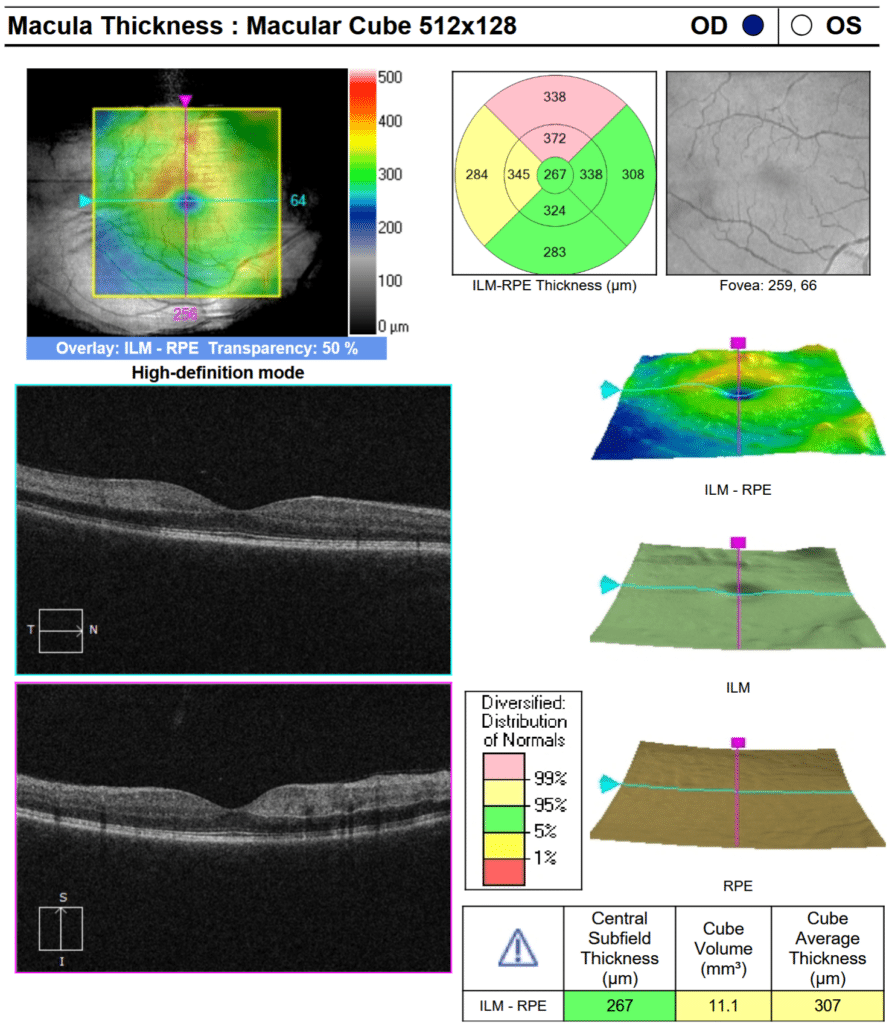
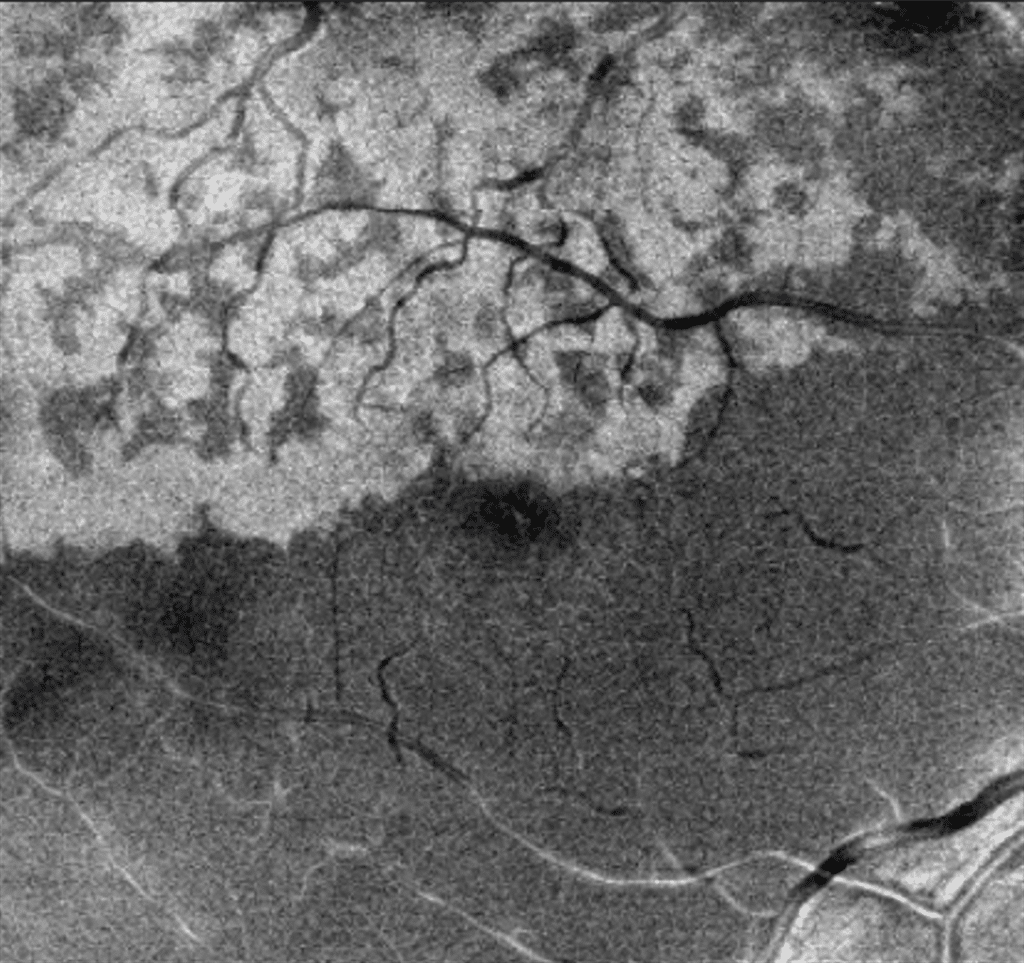
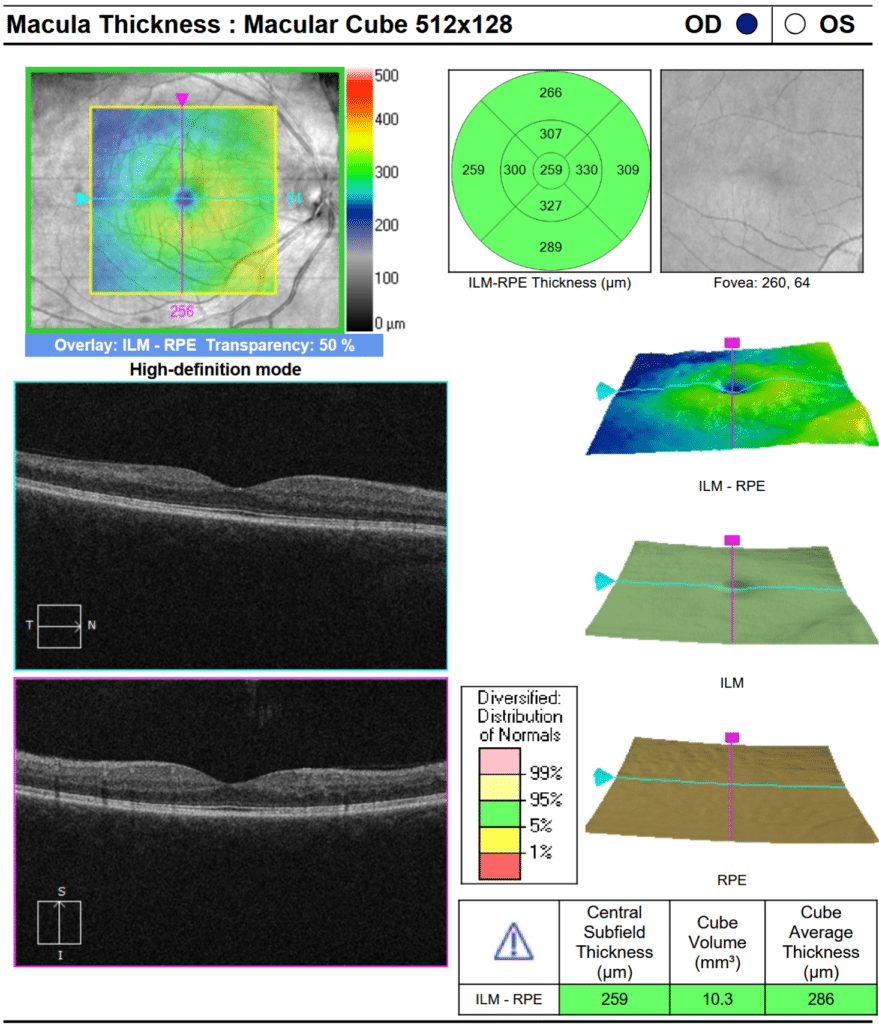
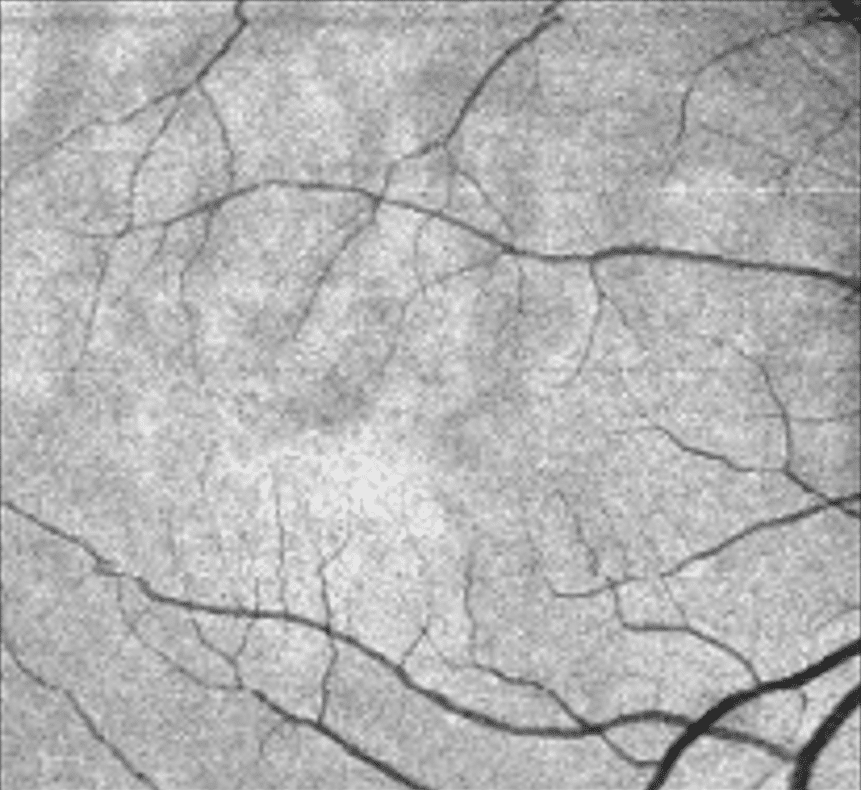
A healthy 43-year-old woman presented to the emergency department with sudden vision loss in her right eye. Ophthalmic examination revealed a visual acuity of 20/32 OD, 20/20 OS, and a normal anterior segment. Dilated fundus examination revealed diffuse venous dilation and tortuosity with associated intraretinal hemorrhage, indicative of a central retinal vein occlusion. Macular examination also revealed subtle retinal whitening localized to the superior aspect of the fovea. Cross-sectional spectral-domain OCT of the central macula revealed multifocal hyperreflectivity within the inner and middle retinal layers in a skip pattern with no macular edema, suggestive of paracentral acute middle maculopathy (PAMM) (see Figure 1). En face OCT angiography demonstrated the presence of a fern-like pattern of hyperreflectivity along the venules (see Figure 2). A follow-up examination one month later revealed attenuation of the PAMM lesions with inner nuclear layer thinning (see Figure 3,4).
In eyes with retinal vascular occlusion, PAMM can present in three morphological patterns – fern-like, globular, or arteriolar.1 The fern-like pattern is visualized with structural en face OCT and characteristically shows band-like hyperreflective lesions at the level of the inner nuclear layer in a perivenular distribution with periarteriolar sparing. Recent advances in the understanding of the inner and middle retinal microvasculature help explain why this pattern occurs. Venous flow through the deep capillary plexus, which is found at the outer limit of the inner nuclear layer, occurs radially through horizontal venules converging into a central vortex venule which then ascends to superficial retinal veins.2 Henceforth, in cases of increased resistance to venous outflow, greater hydrostatic pressure produces the greatest ischemia in the distal end of the deep capillary plexus, rendering the inner nuclear layer most vulnerable to ischemia. The hyperreflectivity seen on OCT is an indication of infarction caused by ischemia to the deep capillary plexus.
Perivenular PAMM has been classically described in the setting of retinal vein occlusions. Although it is considered to represent a milder ischemic insult when compared to other patterns, perivenular PAMM can progress to globular PAMM and even to incomplete retinal artery occlusions.1,3 Accordingly, patients with this clinical picture should be followed closely for progression. In any case of vascular occlusion, OCT angiography coupled with structural en face OCT are invaluable tools in highlighting patterns of ischemia that can be missed or inadequately characterized with either cross-sectional OCT or traditional dye-based angiography alone.4
References:
1. Bakhoum MF, Freund KB, Dolz-Marco R, et al. Am J Ophthalmol. 2018 Nov;195:143-153. doi: 10.1016/j.ajo.2018.07.031.
2. Abtahi SH, Nourinia R, Mazloumi M, et al. Surv Ophthalmol. 2023 May-Jun;68(3):380-387. doi: 10.1016/j.survophthal.2022.11.009.
3. Iyer PG, Swaminathan SS, Trivizki O, et al. Am J Ophthalmol Case Rep. 2021;22:101047. doi: 10.1016/j.ajoc.2021.101047.
4. Zhao PY, Johnson MW, McDonald HR, Sarraf D. Paracentral Acute Middle Maculopathy and the Ischemic Cascade: Toward Interventional Management. AJO. 2022;234:15-19. doi: doi.org/10.1016/j.ajo.2021.07.030.