Department of Ophthalmology, QEII Hospital, Dalhousie University, Halifax, Nova Scotia
A 65-year-old gentleman was referred to the retina service with a 10-year history of nyctalopia and bilateral pigmentary retinal changes, thought to be in keeping with retinitis pigmentosa (RP). Past ocular history was significant only for foreign body. There was no family history of RP.
Examination revealed a best-corrected visual acuity of 6/7.5-1 and 6/6-2 in the right and left eyes, respectively. Intraocular pressures were 17 and 18 in the right and left eyes, respectively. Slit lamp examination demonstrated deep and quiet anterior chambers OU. Dilated fundus examination revealed retinal atrophy with pigment clumping in the mid-peripheral retina bilaterally sparing the fovea and nasal retina.
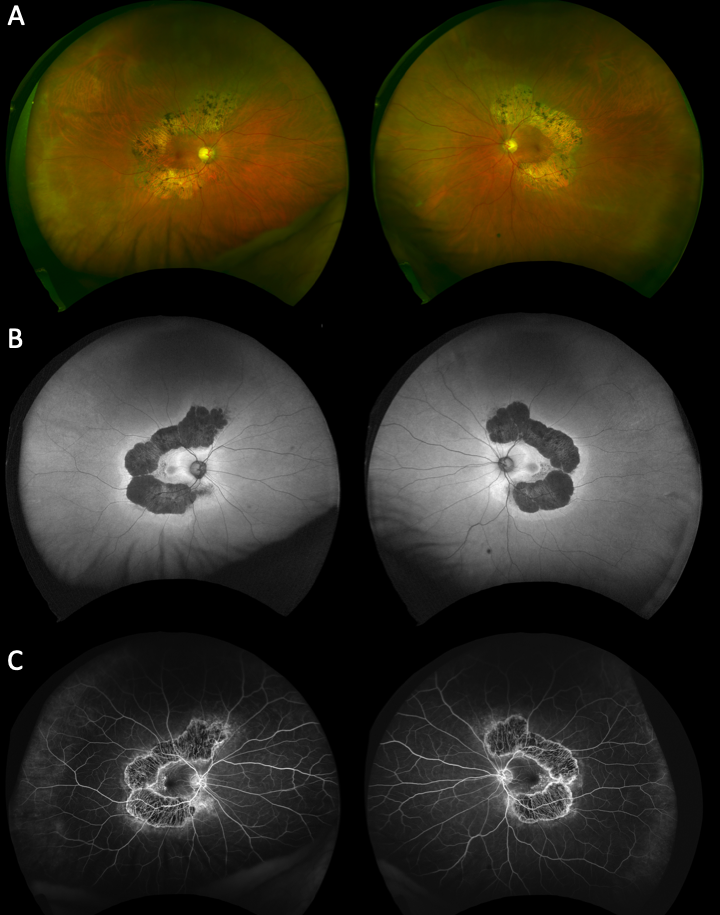
Optical coherence tomography showed thinning of the right optic nerve and slight thinning of left superior optic nerve, maculae were within normal limits. Goldmann and Humphrey 24-2 visual fields revealed partial ring scotomas, sparing the temporal visual fields bilaterally. Ultra-widefield pseudocolour imaging (Figure 1A), fundus autofluorescence (Figure 1B), and fluorescein angiography (Figure 1C) demonstrated findings in keeping with a diagnosis of posterior annular choroidal dystrophy.
Posterior annular choroidal dystrophy (PACD) is a rare disease characterized by annular patterned atrophy of the retinal pigment epithelium and choriocapillaris surrounding the optic nerve and vascular arcades1,2,3. Case reports have shown that patients with PACD commonly present with painless reduced visual acuity worsened by dim lighting4. Although our patient presented with hemispheric atrophy, some reports indicate that hemispheric atrophy may progress to annular atrophy if monitored through long-term follow-up4.
1 Del Valle-Nava F, Sánchez-Ramos J, Hernández-Vázquez A, Gonzalez-Saldivar G, Ramirez-Estudillo A. Posterior polar annular choroidal dystrophy association with cystoid macular edema. Clin Case Reports. 2019;7(2):389-390. Doi:10.1002/ccr3.1967
2 Dikkaya F, Özsütçü M, Özbek M, Erdur SK, Şentürk F. Posterior polar central choroidal dystrophy: A case report. Turkish J Ophthalmol. 2017;47(5):298-301. Doi:10.4274/tjo.56873
3 E de Carlo T, Adhi M, Salz DA, et al. Analysis of Choroidal and Retinal Vasculature in Inherited Retinal Degenerations Using Optical Coherence Tomography Angiography Talisa. Ophthalmic Surg Lasers Imaging Retin. 2016;47(2):120-127. Doi:10.13928/23258160-20160126-04
4 Narayanan R. Posterior polar annular and hemispheric choroidal and retinal dystrophy: Optical coherence tomographic angiography description of a rare case. Indian J Ophthalmol. 2018;66(12):1874. Doi:10.4103/ijo.IJO_367_18