University of Alberta
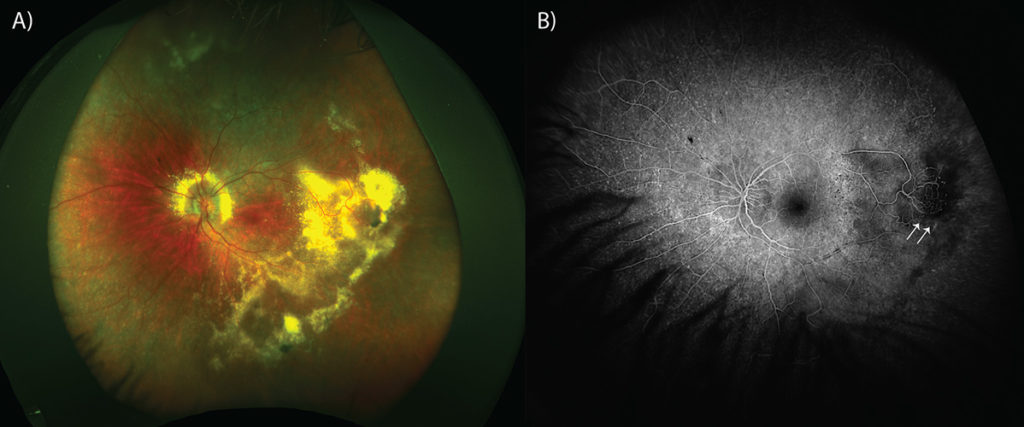
A 12-year old Caucasian female was referred with decreased vision OS. Her past ocular history was remarkable for retinitis pigmentosa, a diagnosis shared by her father. Review of systems and social history were non-contributory. She was not taking any medications. Examination revealed a best-corrected visual acuity of 20/60 OD, and 20/150 OS. Anterior segment examination was revealed posterior subcapsular cataract and trace vitreous cell OU. Fundus examination demonstrated small punctate, whitish lesions scattered throughout the fundus OU consistent with their diagnosis of retinitis pigmentosa. A yellowish retinal mass with a moderately dilated feeding artery and vein was noted in the temporal periphery OS (figure 1a). This lesion was surrounded by exudates. There were exudates surrounding the optic nerve. The presence of a vascular lesion was confirmed via fluorescein angiography (figure 1b, white arrows). Given these findings the patient was diagnosed with vasoproliferative tumor. The lesion was treated with laser photocoagulation.
Vasoproliferative tumor was first described by Shields et al., 19831. Primary lesions occur in 80 percent of cases with secondary lesions comprising the remaining 20 percent. Recently, Shields demonstrated the association of retinitis pigmentosa and secondary vasoproliferative tumor. Compared with primary lesions, secondary lesions are more often bilateral, affect younger patients, multifocal and associated with worse visual acuity2. Accordingly, the diagnosis of vasoproliferative tumor in a young patient should prompt investigations for an associated ocular condition.
1 Shields, J. A., Decker, W. L., Sanborn, G. E., Augsburger, J. J. & Goldberg, R. E. Presumed Acquired Retinal Hemangiomas. Ophthalmology (1983). doi:10.1016/S0161-6420(83)34389-X
2 Shields, C. L. et al. Retinal vasoproliferative tumors: Comparative clinical features of primary vs secondary tumors in 334 cases. JAMA Ophthalmol. (2013). doi:10.1001/2013.jamaophthalmol.524