Department of Ophthalmology and Visual Sciences, Dalhousie University
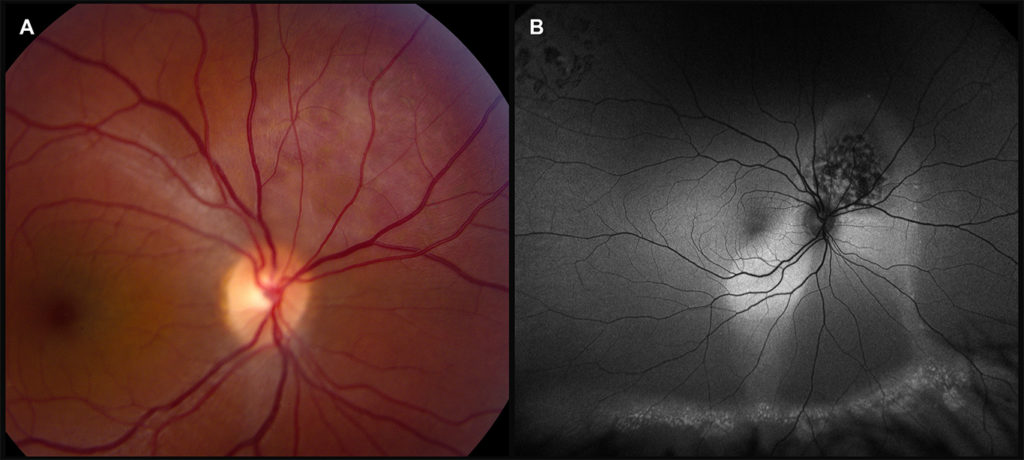
A 35-year-old female was referred from for a 6-month history of a central scotoma and peripapillary edema in her right eye. Ocular history was significant for a retinal tear treated with laser retinopexy in the right eye 3 months prior. Corrected visual acuity was 6/9 in the affected right eye. Right fundus exam showed an oval hypopigmented elevated lesion measuring approximately two disc diameters at the superonasal aspect of optic nerve (Fig. 1A).
Optical coherence tomography (OCT) of the macula showed peripapillary serous retinal detachment (RD) extending to the inferior macula. OCT of the lesion demonstrated a dome-shaped choroidal mass and subretinal fluid. Fluorescein angiography showed early hyperfluorescence with late diffuse staining of the superonasal mass. Fundus autofluorescence showed the hypo-autofluorescent lesion with extensive serous RD (Fig. 1B). B and A-scan ultrasonography demonstrated an elevated mass with high internal reflectivity. Bloodwork was negative for evidence of tumors elsewhere. Based on these findings, a diagnosis of circumscribed choroidal hemangioma with associated serous RD was made. Treatment with photodynamic therapy (PDT) was arranged.
Circumscribed choroidal hemangiomas are rare benign congenital vascular hamartomas of the choroid.1 Most are unilateral and, unlike diffuse choroidal hemangiomas, have no known associated systemic manifestations. Classically, a round orange-red elevated mass in the posterior pole is visible.2,3 However, hemangiomas may blend into the surrounding choroid and make clinical diagnosis difficult.
Multimodal imaging is important to differentiate suspected hemangiomas from other causes of serous RD and choroidal tumors, especially amelanotic choroidal melanoma or metastasis. Ultrasonography shows characteristic high internal reflectivity on A-scan and solid acoustic appearance on B-scan.3 Fluorescein angiography shows early lacy hyperfluorescence, which increases in later phases. Lesions typically do not enlarge but affect vision due to complications including progression of serous RD, photoreceptor degeneration, and cystoid macular edema.3,4 In symptomatic patients, early PDT is the treatment of choice.4,5
1 Karimi S, Nourinia R, Mashayekhi A. Circumscribed Choroidal Hemangioma. J Ophthalmic Vis Res 2015; 10:320-8. https://doi.org/10.4103/2008-322X.170353.
2 Krohn J, Rishi P, Frøystein T, Singh AD. Circumscribed choroidal haemangioma: clinical and topographical features. Br J Ophthalmol 2019; 103:1448-52. https://doi.org/10.1136/bjophthalmol-2018-313388.
3 Shields CL, Honavar SG, Shields JA, Cater J, Demirci H. Circumscribed choroidal hemangioma: clinical manifestations and factors predictive of visual outcome in 200 consecutive cases. Ophthalmology 2001; 108:2237-48. https://doi.org/10.1016/s0161-6420(01)00812-0.
4 Mashayekhi A, Shields CL. Circumscribed choroidal hemangioma. Curr Opin Ophthalmol 2003; 14:142-9. https://doi.org/10.1097/00055735-200306000-00006.
5 Lee J, Lee CS, Kim M et al. Retinal fluid changes and therapeutic effects in symptomatic circumscribed choroidal hemangioma patients: a long-term follow up study. BMC Ophthalmol 2018; 18:321. https://doi.org/ 10.1186/s12886-018-0993-x.