Southern Alberta Eye Center, Rockyview Hospital, University of Calgary
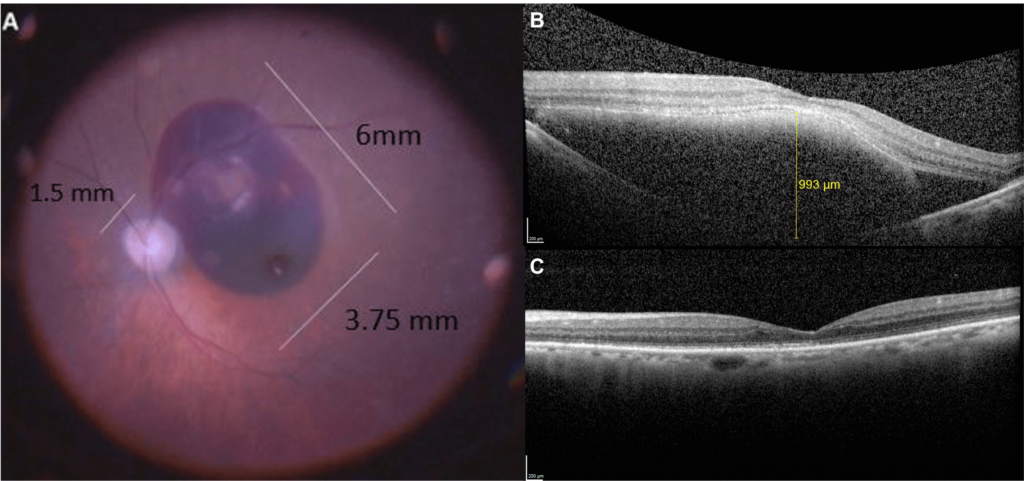
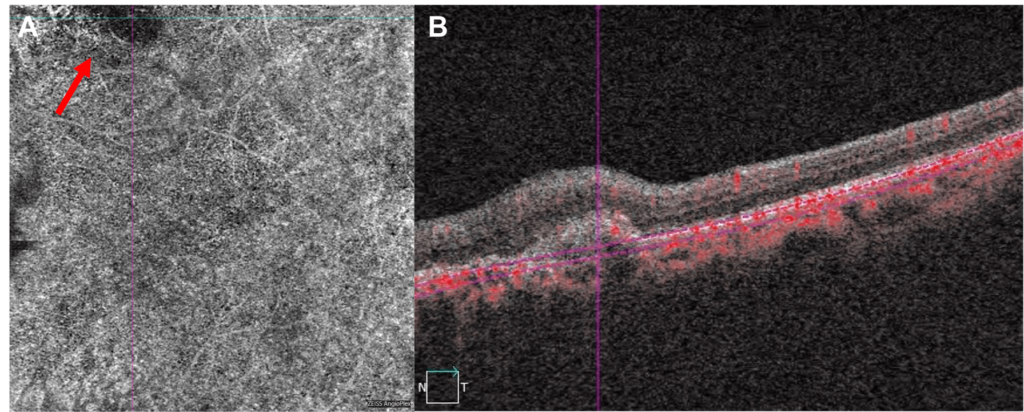
84-year-old male with age related macular degeneration (ARMD) presented 5 days after suddenly losing central vision OS. Medical history was significant for hypertension and benign prostate hypertrophy. Best corrected visual acuity (BCVA) measured 20/30 OD and counting fingers OS. Anterior segments were unremarkable except for PCIOL OU. A large submacular hemorrhage (SMH) OS was visualized measuring 6.0 x 3.75 x 1.0 mm (Figure 1). Macular optical coherence tomography (OCT) revealed thickening with hyper & hyporeflective subretinal material (Figure 1B). Preoperative intravitreal bevacizumab (IVB) and subsequent vitrectomy surgery was performed with subretinal tissue plasminogen activator (rTPA) delivery and gas exchange. BCVA improved to 20/60 two months postoperatively with resolution of the hemorrhage and some resultant thinning and irregularity in the outer nuclear and ellipsoid photoreceptor layers (Figure 1C). Regular IVB was continued postoperatively for the extrafoveal macular neovascularization (MNV) process (Figure 2).
SMH is an important complication that can occur in patients with ARMD.1 Damage to the photoreceptors and retinal pigment epithelium (RPE) layers can occur from iron-induced toxicity. The irreversible nature of this retinal injury is time-dependent.2,3 There are a variety of treatment options, including anti-VEGF therapy, pneumatic displacement, rTPA, and vittrectomy.4 rTPA is the main enzyme responsible for the transformation of plasminogen into plasmin and clot break down. Many studies have reported significant improvement in vision following treatment of SMH with rTPA.5 Our case combines these various modalities to treat both the subretinal bleeding and MNV process.
1 Ochinciuc R, Balta F, Branisteanu D, et al. Subretinal alteplase injections in massive subretinal hemorrhage due to age‑related macular degeneration: A case report series. Exp Ther Med. 2020;20(6):1-1. doi:10.3892/etm.2020.9338
2 Lee JH, Lee MY, Lee WK. Incidence and risk factors of massive subretinal hemorrhage in retinal angiomatous proliferation. Hartnett ME, ed. PLoS One. 2017;12(10):e0186272. doi:10.1371/journal.pone.0186272
3 Maranduca MA, Branisteanu D, Serban DN, et al. Synthesis and physiological implications of melanic pigments (review). Oncol Lett. 2019;17(5):4183-4187. doi:10.3892/ol.2019.10071
4 Management of Submacular Hemorrhage - American Academy of Ophthalmology. https://www.aao.org/eyenet/article/management-of-submacular-hemorrhage. Accessed January 22, 2021.
5 Kitagawa Y, Shimada H, Mori R, Tanaka K, Yuzawa M. Intravitreal Tissue Plasminogen Activator, Ranibizumab, and Gas Injection for Submacular Hemorrhage in Polypoidal Choroidal Vasculopathy. Ophthalmology. 2016;123(6):1278-1286. doi:10.1016/j.ophtha.2016.01.035